
What you need to know
Slit Lamp Viewing
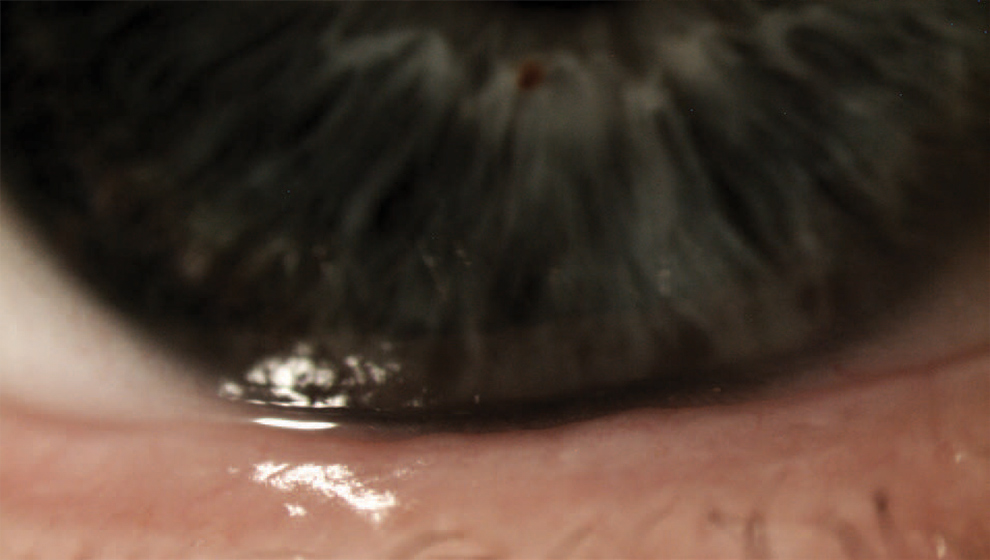
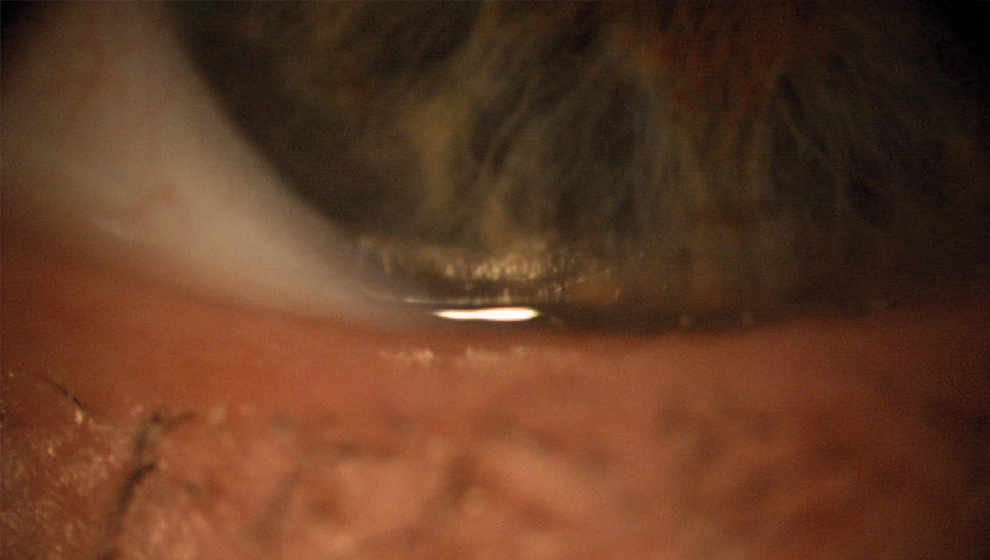
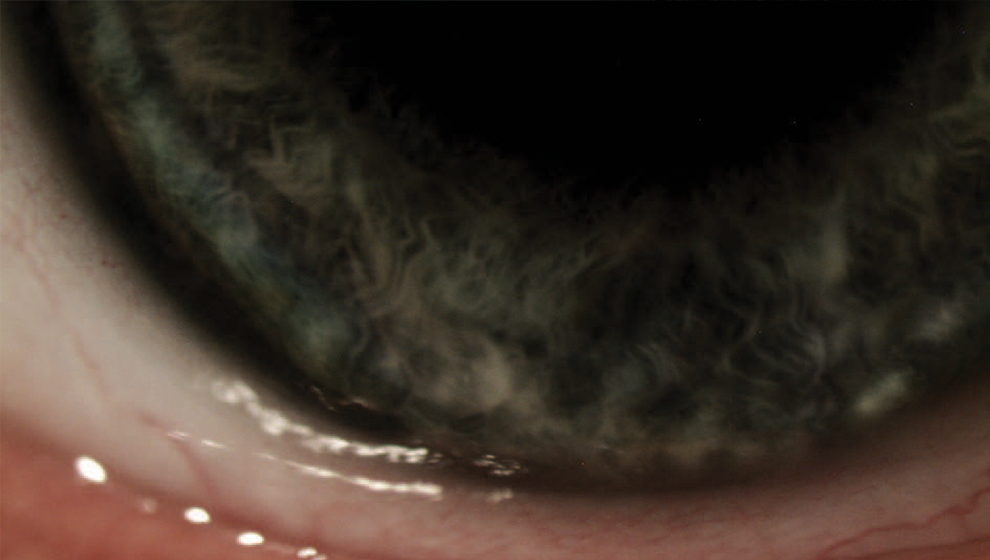
- Narrow slit beam with low intensity to measure (with eye-piece graticule) or grade inferior tear meniscus height in primary gaze and with normal blinking.
- High magnification (40x)
- Direct focal illumination
Grading
Tear meniscus height
Incidence
Questionnaires - such as:
- Standardized Patient Evaluation of Eye Dryness Questionnaire (SPEED)
- Ocular Surface Disease Index (OSDI)
- Contact Lens Dry Eye Questionnaire (CLDEQ)
- CLDEQ-8, McMonnies Dry Eye Index
- Dry Eye Questionnaire (DEQ)
- Non-invasive tests - tear meniscus height (lower lid margin to top of specular reflex) and regularity
- Invasive tests - Schirmer, Phenol red thread. Invasive and non-invasive break-up time, lipid layer presence.
Etiology
- Multifactorial, including age, medication, systemic or ocular conditions, environment
- Contact lens wear interferes with normal tear film structure and function
- Increased tear film evaporation leads to thinning of pre- and post-lens tear layers
Symptoms
- Dryness, discomfort, grittiness, irritation, sensitivity to adverse environments.
Signs
- Reduced tear meniscus height, irregular tear meniscus (notching or scalloped edge), concave tear profile
- Low Schirmer test scores (at 5 mins, normal >10mm, borderline 5-10mm, severe dry <5mm) or low Phenol red thread test scores (at 15 secs, dry eye <10mm)
Patient Recommendations
Recommendations
- Address associated systemic or ocular conditions
- Artificial tear supplements
- Change lens type (RGP to silicone hydrogel), material or wearing schedule (monthly replacement to two weekly)
- Maintain good lens cleaning including rub and rinse step
- Manage all grades if signs or symptoms exist - improve tear film quality
- Change lens care solution to latest generation of products
- Manage any tear quality issues
- Rewetting drops or liposomal sprays
- Attention to nutrition or nutritional supplements (essential fatty acids)
- Tear retention measures (to reduce drainage and increase tear contact time) such as punctal plugs or surgery
- Manage any meibomian gland issues
Prognosis
Generally good resolution of symptoms with appropriate management unless intractable underlying systemic or ocular condition
